December 2, 2022
New Reference Values for Measuring Tongue Pressure to Predict the Development of Aspiration Pneumonia after Ventilator Withdrawal in Elderly




Key Points:
- The study showed that the predictive accuracy of feeding and swallowing dysfunction after ventilator weaning improved with the addition of tongue pressure measurements.
- In Japan, there have been no reports of tongue pressure measurements after ventilator weaning, and this is the first reference value for maximum tongue pressure. It is expected to be applicable for the initiation of oral intake after ventilator management because of COVID-19 infection.
- The use of maximal tongue pressure values combined with conventional swallowing assessments when initiating oral intake for patients after weaning from a ventilator can help prevent the development of aspiration pneumonia.
Summary:
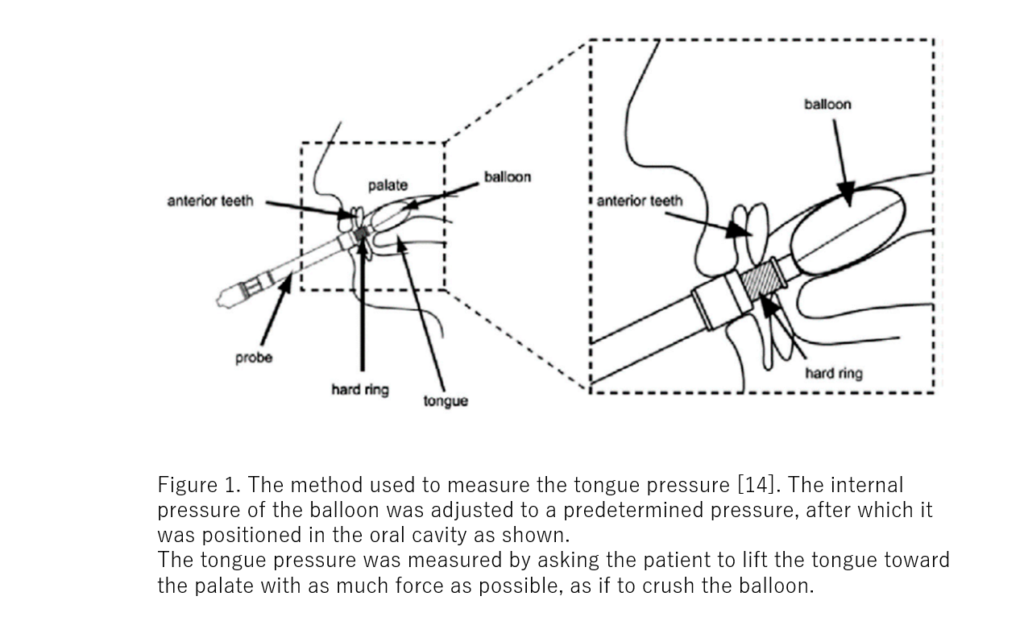
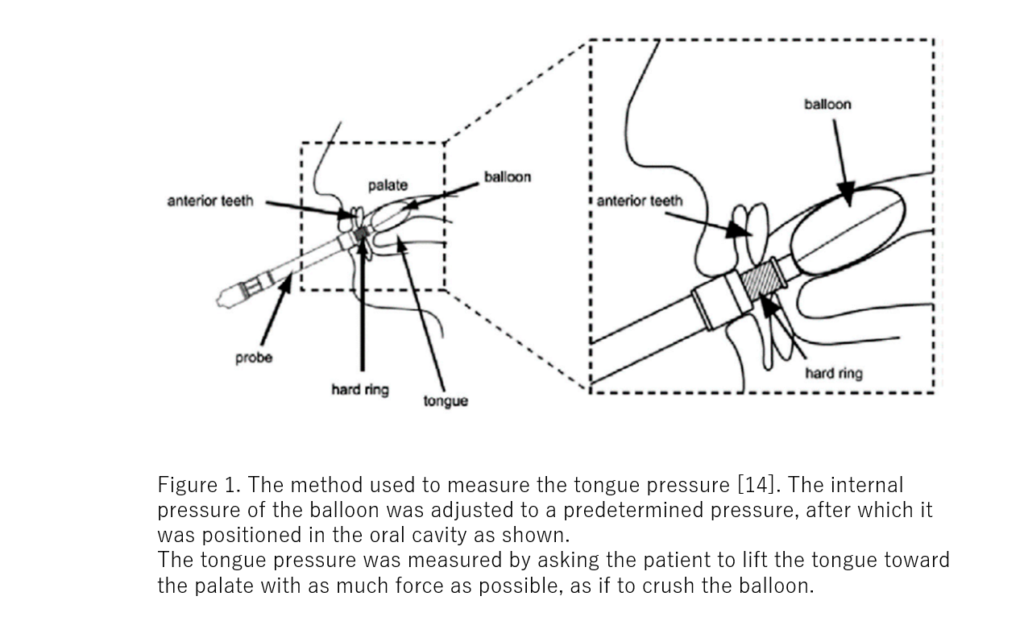
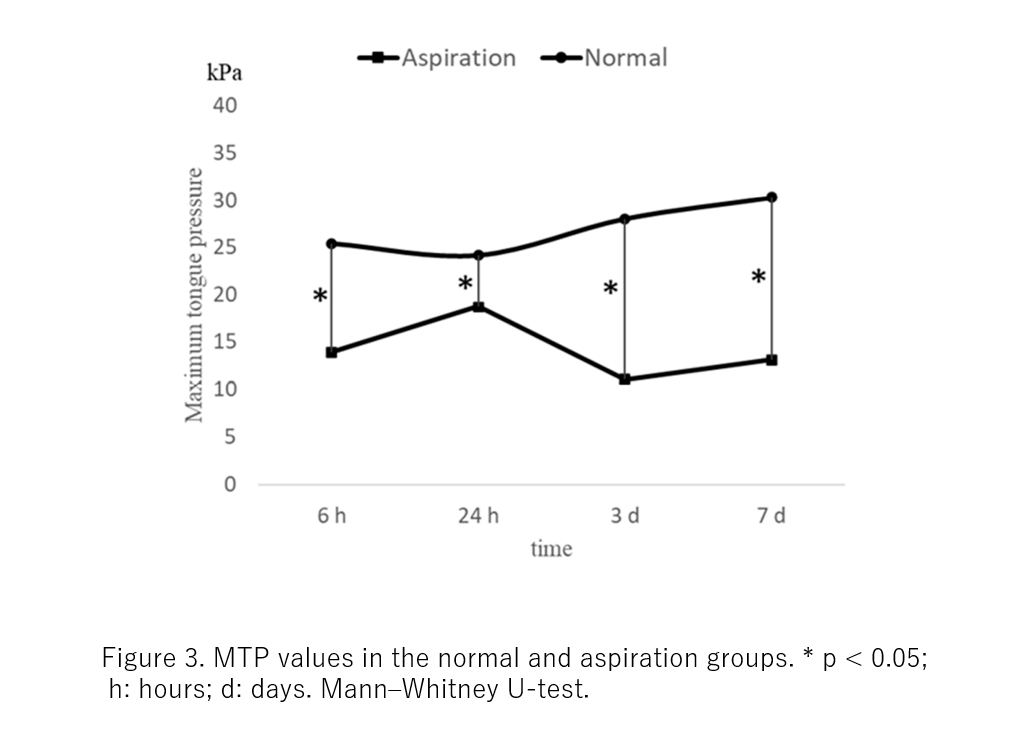
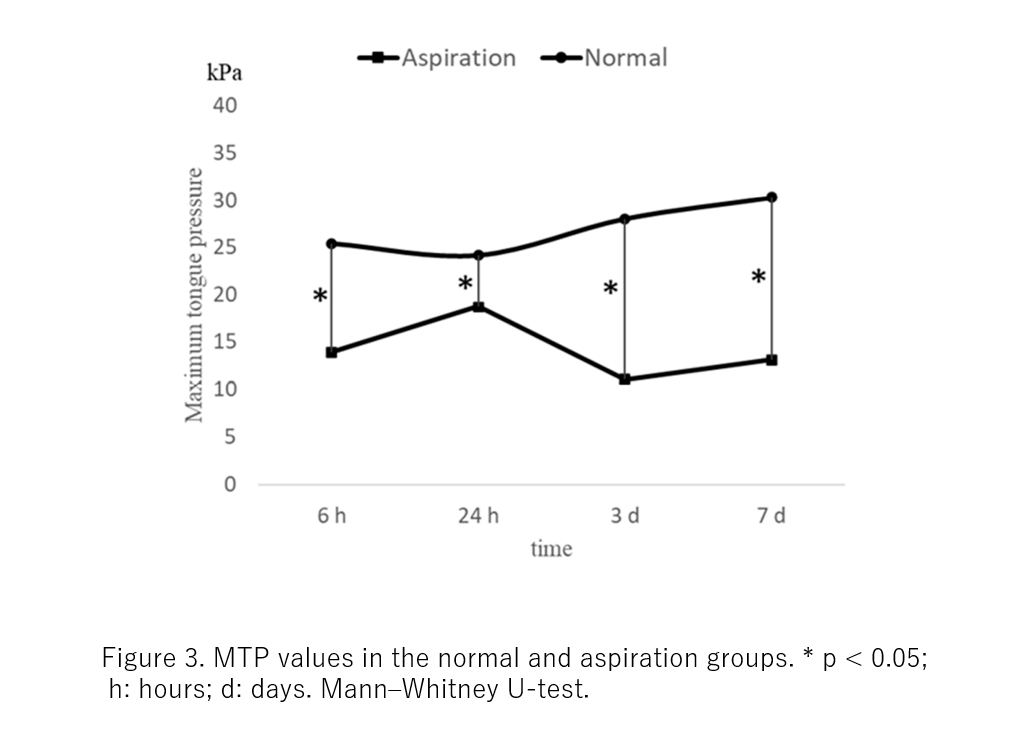
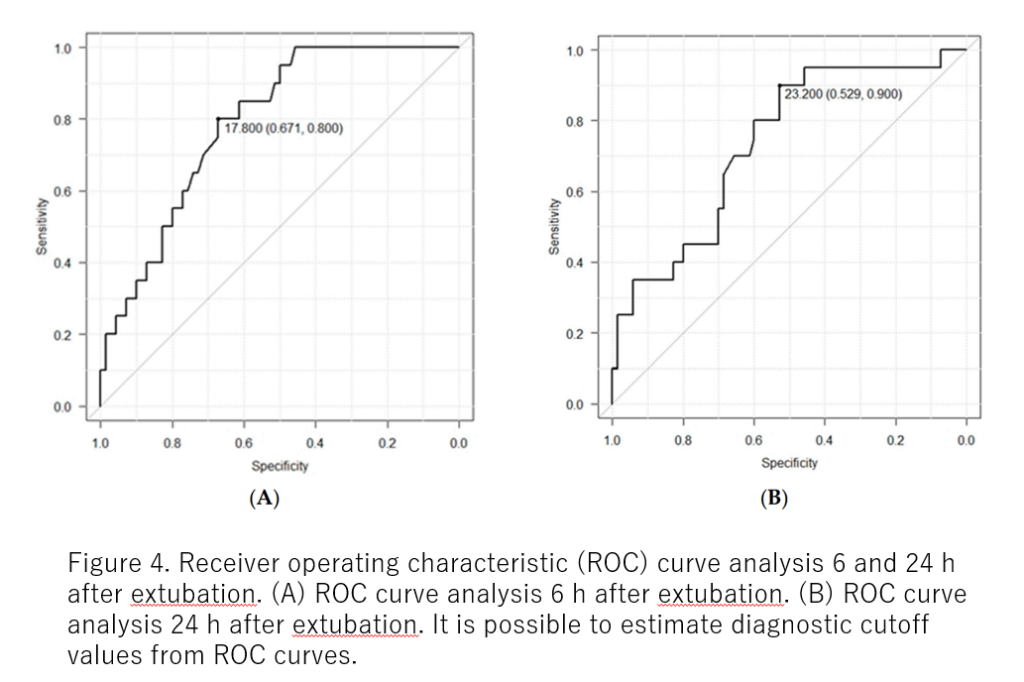
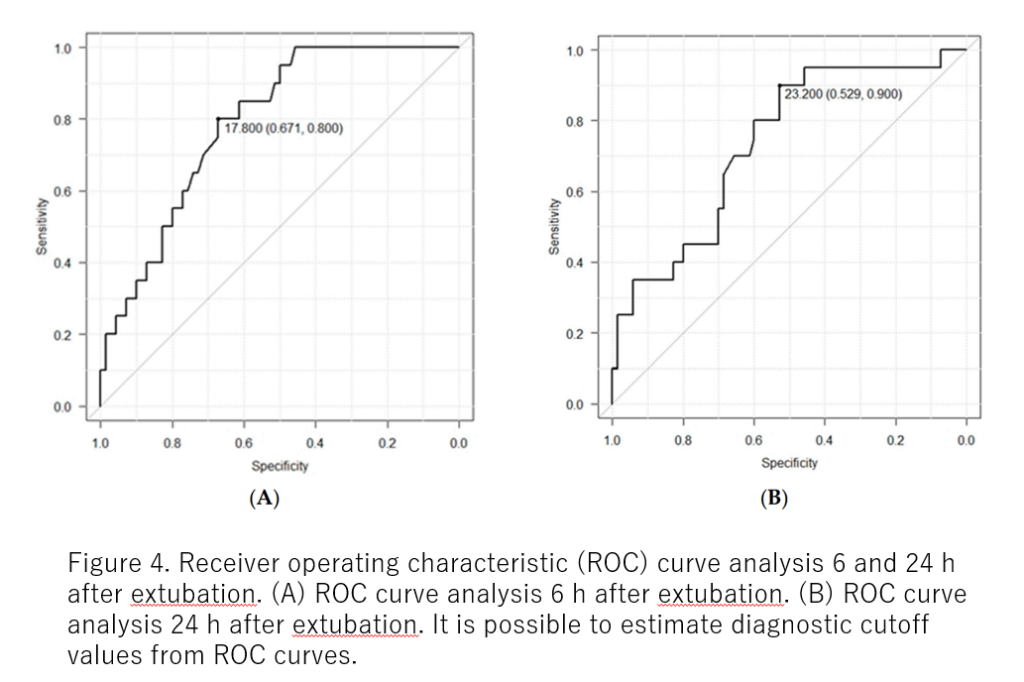
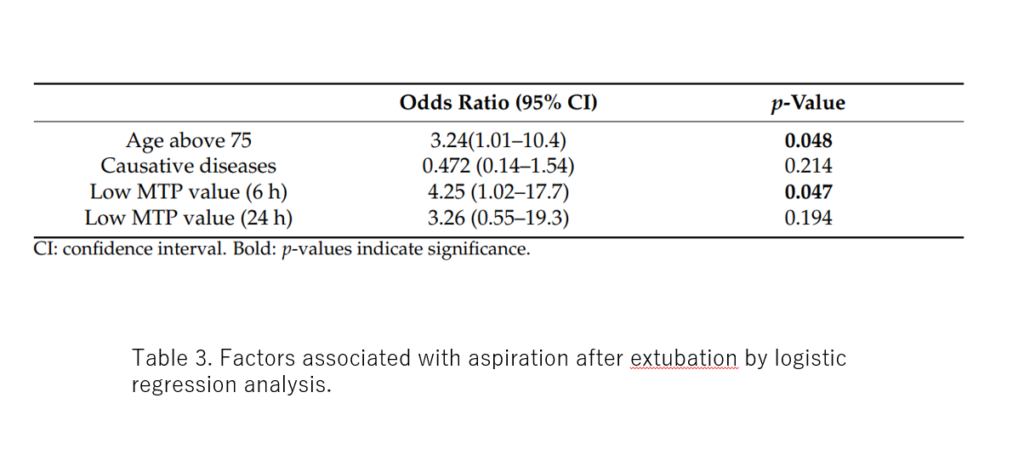
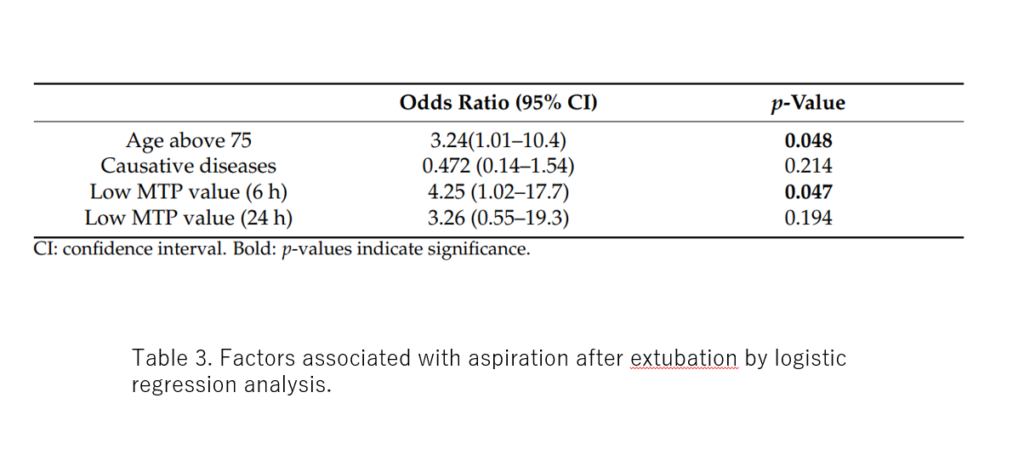
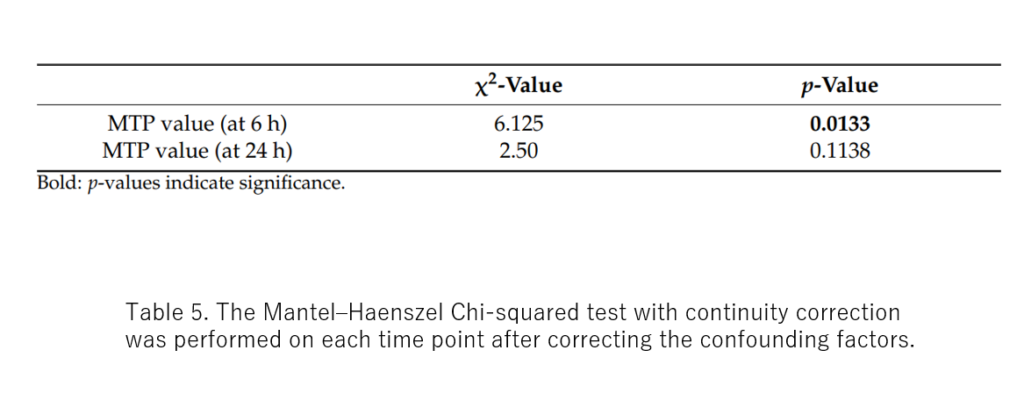
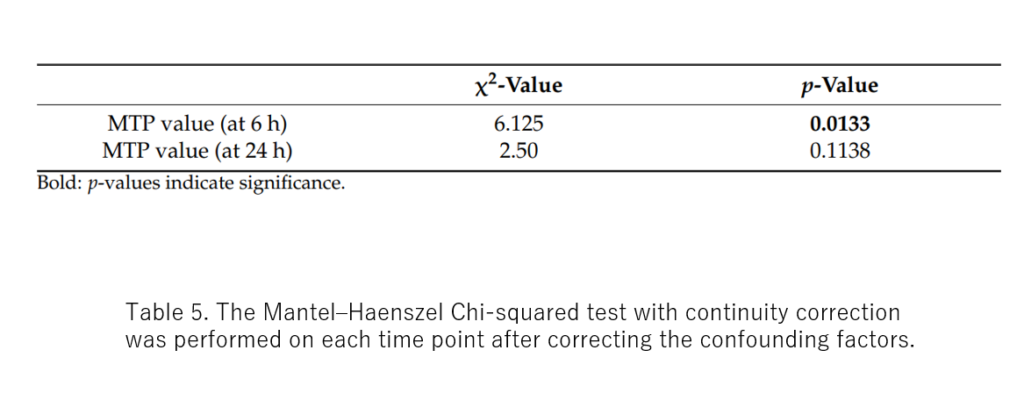
Approximately 50% of ventilator-assisted patients experience a temporary decline in swallowing function and, depending on the situation, may be affected by aspiration pneumonia on resuming eating. Even if the underlying disease improves, aspiration pneumonia may develop, resulting in re-installation of a ventilator, prolonged hospitalization, and other adverse effects. The presence of dysphagia can be confirmed by multiple screening tests, such as the repeated saliva swallow and water swallow tests. However, aspiration still occurs in <20% of the patients even though the screening tests show no presence of dysphagia, resulting in aspiration pneumonia. Maximal tongue pressure values have been reported to reflect swallowing function. In this study, measuring the maximal tongue pressure in patients after weaning from the ventilator provided new reference values that may reduce these adverse events. The study included 90 patients and measured the maximum tongue pressure values at 6 h and 24 h after ventilator withdrawal. These 90 patients were divided into two groups: the normal group, who did not aspirate, and the aspiration group, who were older than the normal group. Lower maximum tongue pressure values at 6 h and 24 h were associated with the development of aspiration in patients. In patients aged >75 years, a diagnostic cutoff maximum tongue pressure value of 17.8 kPa could be used as the basis for determining the risk of aspiration. Therefore, the study has shown that it is extremely useful to measure the maximal tongue pressure value after weaning from the ventilator before considering oral intake. The results also provide a possible standard for determining the need for feeding and swallowing rehabilitation after weaning from the ventilator and making changes through the patients’ diet prior to undertaking life-saving measures.
Approximately 50% of ventilator-assisted patients experience a temporary decline in swallowing function and, depending on the situation, may be affected by aspiration pneumonia on resuming eating. Even if the underlying disease improves, aspiration pneumonia may develop, resulting in re-installation of a ventilator, prolonged hospitalization, and other adverse effects. The presence of dysphagia can be confirmed by multiple screening tests, such as the repeated saliva swallow and water swallow tests. However, aspiration still occurs in <20% of the patients even though the screening tests show no presence of dysphagia, resulting in aspiration pneumonia. Maximal tongue pressure values have been reported to reflect swallowing function. In this study, measuring the maximal tongue pressure in patients after weaning from the ventilator provided new reference values that may reduce these adverse events. The study included 90 patients and measured the maximum tongue pressure values at 6 h and 24 h after ventilator withdrawal. These 90 patients were divided into two groups: the normal group, who did not aspirate, and the aspiration group, who were older than the normal group. Lower maximum tongue pressure values at 6 h and 24 h were associated with the development of aspiration in patients. In patients aged >75 years, a diagnostic cutoff maximum tongue pressure value of 17.8 kPa could be used as the basis for determining the risk of aspiration. Therefore, the study has shown that it is extremely useful to measure the maximal tongue pressure value after weaning from the ventilator before considering oral intake. The results also provide a possible standard for determining the need for feeding and swallowing rehabilitation after weaning from the ventilator and making changes through the patients’ diet prior to undertaking life-saving measures.
Journal
Journal of Clinical Medicine November 7 2022 issue
Title
Use of Maximum Tongue Pressure Values to Examine the Presence of Dysphagia after Extubation and Prevent Aspiration Pneumonia in Elderly Emergency Patients
Authors
Ryo Ichibayashi, Hideki Sekiya, Kosuke Kaneko, Mitsuru Honda
DOI No.
doi.org/10.3390/jcm11216599
Journal of Clinical Medicine November 7 2022 issue
Title
Use of Maximum Tongue Pressure Values to Examine the Presence of Dysphagia after Extubation and Prevent Aspiration Pneumonia in Elderly Emergency Patients
Authors
Ryo Ichibayashi, Hideki Sekiya, Kosuke Kaneko, Mitsuru Honda
DOI No.
doi.org/10.3390/jcm11216599
READ MORE RESEARCH NEWS - MEDICINE
ACADEMICS
Undergraduate Programs
– Medicine
– Pharmaceutical Sciences
– Science
– Nursing
– Health Science
Graduate Programs
–Medicine
–Pharmaceutical Sciences
–Science
–Nursing
Undergraduate Programs
– Medicine
– Pharmaceutical Sciences
– Science
– Nursing
– Health Science
Graduate Programs
–Medicine
–Pharmaceutical Sciences
–Science
–Nursing
RESEARCH
– News
– Guidelines & Policies
– Support Offices
– Facilities
– Security Export Control
Non-Degree Programs
– Clinical Elective Program
– International Physician Observership Program