January 26, 2024
App enhances nurses' care coordination competency for critically ill patients
Receiving objective feedback on care coordination competencies strengthens the development of care coordination behaviors




Key Highlights:
- The group that engaged in self-assessment and received feedback through the NCCCS app demonstrated an increase in the frequency of care coordination behaviors after one month, in contrast to the self-assessment group without feedback. Notably, the participants with less experience in managing critically ill patients did not exhibit a corresponding increase in the frequency of these behaviors.
- The group, whose NCCCS score was below the national average as of 2017 experienced an increased frequency of care coordination behaviors one month later, following feedback from the NCCCS app, compared to the group without feedback.
- The group receiving feedback on their self-assessment scores through the NCCCS app exhibited heightened attention, confidence, and interest in learning about care coordination, in contrast to the group without feedback. Additionally, they reported that the use of the NCCCS app fostered teamwork and enhanced the quality of care.
- The findings of this study may provide a new strategy for improving outcomes in critically ill patients on life support.
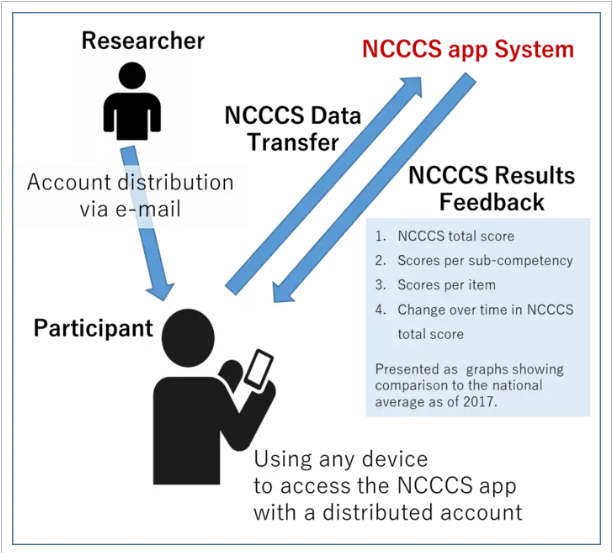
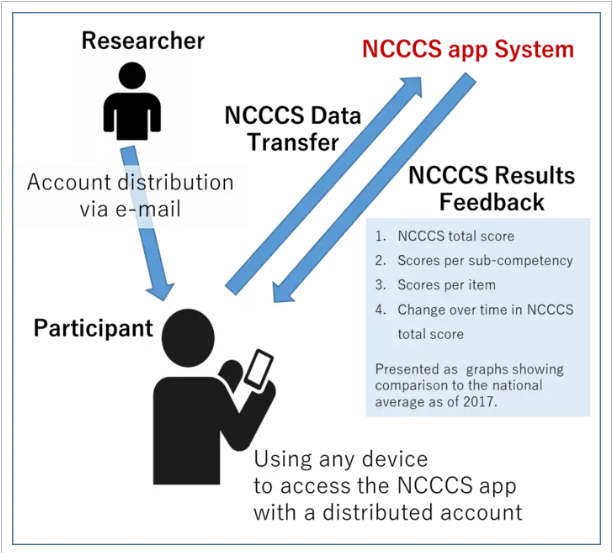
THE RESEARCHER DISTRIBUTED NCCCS APP ACCOUNTS VIA EMAIL, ALLOWING PARTICIPANTS TO ACCESS THE APP ON ANY DEVICE. FEEDBACK, PRESENTED IN GRAPHICAL FORM, INCLUDED PARTICIPANTS’ NCCCS TOTAL SCORES, SUB-COMPETENCY SCORES, AND BEHAVIORAL LEVEL ITEM SCORES. THIS VISUAL REPRESENTATION FACILITATED A COMPARISON OF PARTICIPANTS’ SCORES WITH THE 2017 NATIONAL AVERAGE.
Journal
Japan Journal of Nursing Science
DOI No.
10.1111/jjns.12584
Method of Research
Data/statistical analysis
Subject of Research
People
Article Title
Effectiveness of a self-assessment application in evaluating the care coordination competency of intensive care unit nurses in managing patients on life support: An intervention study
EurekAlert!
Japan Journal of Nursing Science
DOI No.
10.1111/jjns.12584
Method of Research
Data/statistical analysis
Subject of Research
People
Article Title
Effectiveness of a self-assessment application in evaluating the care coordination competency of intensive care unit nurses in managing patients on life support: An intervention study
EurekAlert!
READ MORE RESEARCH NEWS - Nursing
ACADEMICS
Undergraduate Programs
– Medicine
– Pharmaceutical Sciences
– Science
– Nursing
– Health Science
Graduate Programs
–Medicine
–Pharmaceutical Sciences
–Science
–Nursing
Undergraduate Programs
– Medicine
– Pharmaceutical Sciences
– Science
– Nursing
– Health Science
Graduate Programs
–Medicine
–Pharmaceutical Sciences
–Science
–Nursing
RESEARCH
– News
– Guidelines & Policies
– Support Offices
– Facilities
– Security Export Control
Non-Degree Programs
– Clinical Elective Program
– International Physician Observership Program