May 10, 2021
Developing an AI model for pathological diagnosis of testicular tissue in male infertility using image recognition AI that requires no programming
~ You don’t need to be an engineer to build an AI

Key points of the research
- Ito et al. developed a novel automatic diagnosis system for testicular histopathology in male patients with infertility using image recognition artificial intelligence (AI) that requires no programming.
- They built an AI model using machine learning and deep learning without having advanced expertise.
- It is expected that AI models in medicine will be developed using services that can easily utilize AI, which was previously thought to be a barrier to its widespread introduction.
(1) Background
Approximately half of the causes of infertility are due to problems on the male side. Among these, azoospermia is the most serious. There are two types of azoospermia: obstructive azoospermia and non-obstructive azoospermia. Both types of azoospermia require intratesticular sperm extraction (TESE) to extract sperm. During this procedure, a portion of testicular tissue is submitted as a pathology specimen to ascertain the condition of inside the testicle, and a pathologist quantifies the condition inside the testicle using the Johnsen scoring method. In the case of obstructive azoospermia, the proportion of sperm recovered is high, and the Johnsen score is often 8 points or higher. However, in non-obstructive azoospermia, the rate of sperm retrieval tends to be low, with a Johnsen score of 1–3 points. The research group has started to develop a testicular pathology AI model that identifies the Johnsen score from testicular pathology images using a machine learning approach. Originally, it was difficult to create an AI model unless you were an engineer with expertise in AI. However, by using Google Cloud’s AutoML Vision, it is now possible to build AI models without advanced expertise. The research group succeeded in developing the AI model at the initiative of doctors without the help of engineers.
Approximately half of the causes of infertility are due to problems on the male side. Among these, azoospermia is the most serious. There are two types of azoospermia: obstructive azoospermia and non-obstructive azoospermia. Both types of azoospermia require intratesticular sperm extraction (TESE) to extract sperm. During this procedure, a portion of testicular tissue is submitted as a pathology specimen to ascertain the condition of inside the testicle, and a pathologist quantifies the condition inside the testicle using the Johnsen scoring method. In the case of obstructive azoospermia, the proportion of sperm recovered is high, and the Johnsen score is often 8 points or higher. However, in non-obstructive azoospermia, the rate of sperm retrieval tends to be low, with a Johnsen score of 1–3 points. The research group has started to develop a testicular pathology AI model that identifies the Johnsen score from testicular pathology images using a machine learning approach. Originally, it was difficult to create an AI model unless you were an engineer with expertise in AI. However, by using Google Cloud’s AutoML Vision, it is now possible to build AI models without advanced expertise. The research group succeeded in developing the AI model at the initiative of doctors without the help of engineers.
(2) Details
In this study, 275 patients who underwent TESE for obstructive or non-obstructive azoospermia who visited the Reproductive Center of Toho University Omori Medical Center between January 2010 and December 2019 were included. The pathological specimens from 264 out of 275 cases were used, and Johnsen scores 1–3 were classified as label 1, Johnsen scores 4–5 as label 2, Johnsen scores 6–7 as label 3, and Johnsen scores 8–10 as label 4 (Fig. 1).
In this study, 275 patients who underwent TESE for obstructive or non-obstructive azoospermia who visited the Reproductive Center of Toho University Omori Medical Center between January 2010 and December 2019 were included. The pathological specimens from 264 out of 275 cases were used, and Johnsen scores 1–3 were classified as label 1, Johnsen scores 4–5 as label 2, Johnsen scores 6–7 as label 3, and Johnsen scores 8–10 as label 4 (Fig. 1).
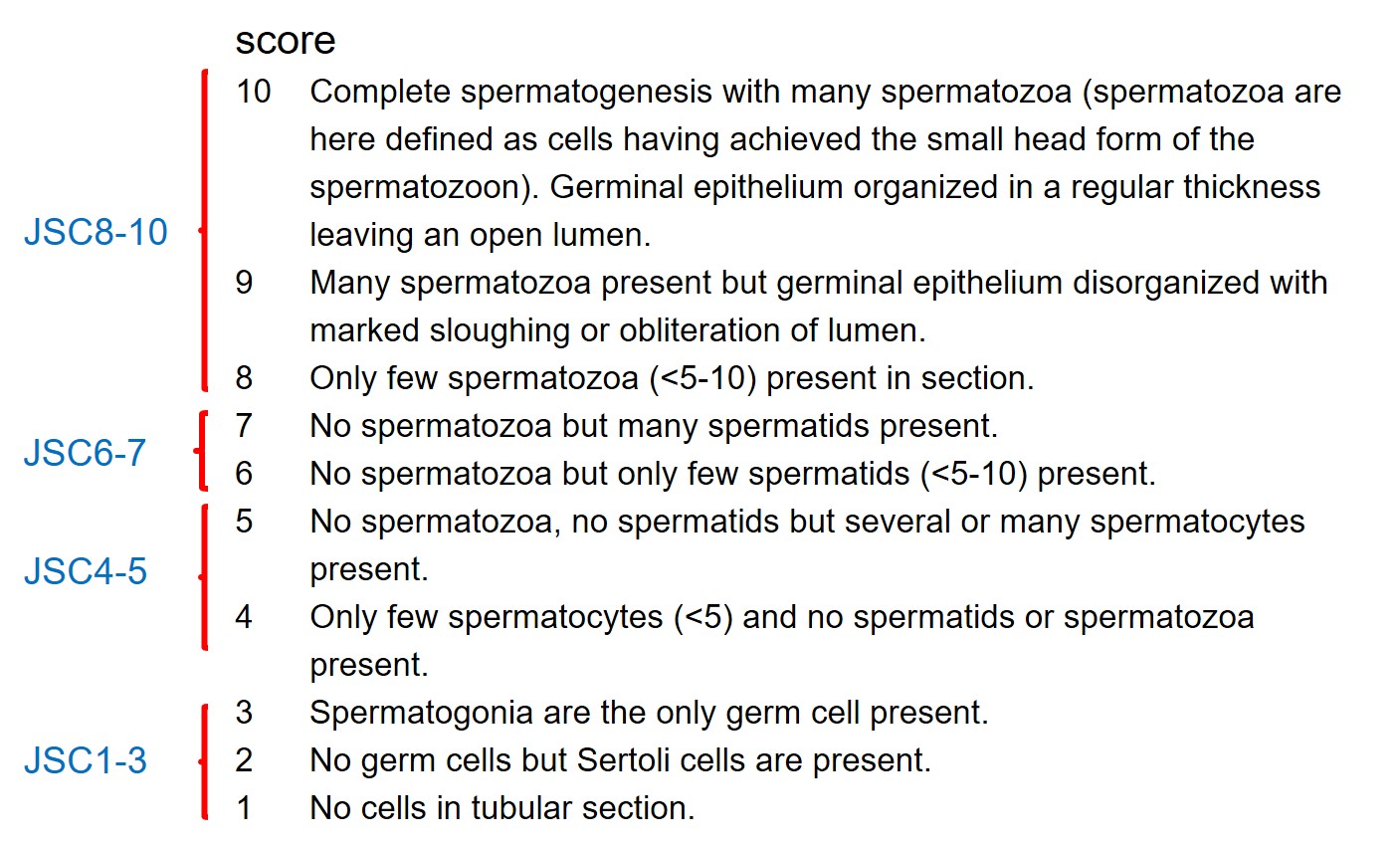
Fig. 1
We obtained a total of 7115 pathological images: 2486 for label 1, 1614 for label 2, 2019 for label 3, and 1036 for label 4 (Fig. 2). The captured images were uploaded to AutoML Vision as training image data. After the upload was complete, clicking on “START TRAINING” started the training process. No advanced AI knowledge was required to build the AI model. Once the model training is completed, the evaluation metrics of the model were automatically created. From these results, it was possible to check the extent of scrutiny. For the developed testicular pathology AI model, the average percent fit (AUC) was 0.826. This indicates a positive test result rate of 82.6% (Fig. 2). In addition, to increase the positive diagnosis rate, they cropped the area to determine the Johnsen score in a single pathology image. A total of 9882 pathological images were cropped: 1483 for label 1, 3437 for label 2, 3523 for label 3, and 1439 for label 4. As in previous studies, they uploaded the data to AutoML Vision to build a testicular pathology AI model. The correct diagnosis rate was 99.5%.
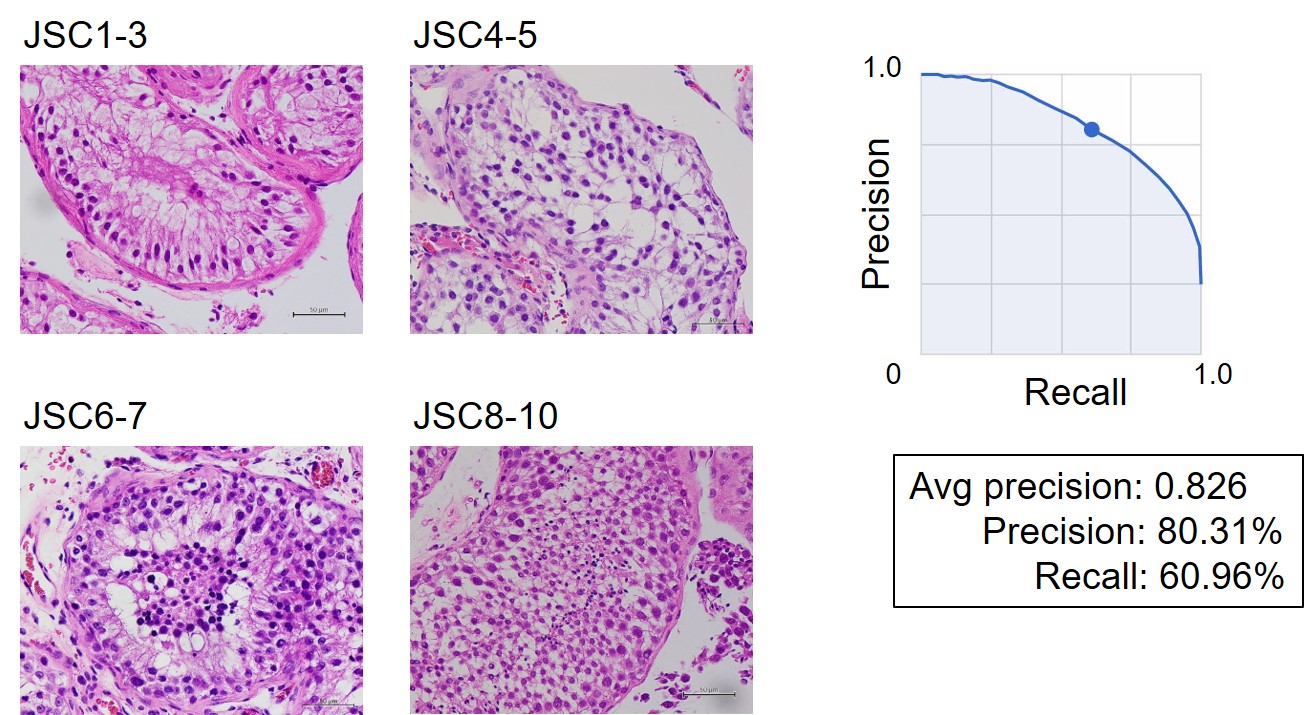
Fig. 2
(3) Social significance and future plans
Currently, the Johnsen score is determined by a pathologist. This research group is the first in the world to develop an AI model for predicting the Johnsen score of testicular pathology. Using this AI model, we can obtain a positive diagnosis rate of more than 80%. Although it cannot replace pathologists immediately, it is expected that a testicular pathology AI model that recognizes the Johnsen score will be established in the future, which is easier to use and has a higher positive diagnosis rate. In addition, by building physician-led AI models, digital advances are expected to rapidly penetrate the medical field in the future.
Currently, the Johnsen score is determined by a pathologist. This research group is the first in the world to develop an AI model for predicting the Johnsen score of testicular pathology. Using this AI model, we can obtain a positive diagnosis rate of more than 80%. Although it cannot replace pathologists immediately, it is expected that a testicular pathology AI model that recognizes the Johnsen score will be established in the future, which is easier to use and has a higher positive diagnosis rate. In addition, by building physician-led AI models, digital advances are expected to rapidly penetrate the medical field in the future.
Journal name
Scientific Reports (Online edition: May 10, 2021)
Title of paper
A method for utilizing automated machine learning for histopathological classification of testes based on Johnsen scores
Author(s)
Yurika Ito, Mami Unagami, Fumito Yamabe, Yozo Mitsui, Koichi Nakajima, Koichi Nagao, Hideyuki Kobayashi* (*Responsible Author)
DOI No. 10.1038/s41598-021-89369-z
Scientific Reports (Online edition: May 10, 2021)
Title of paper
A method for utilizing automated machine learning for histopathological classification of testes based on Johnsen scores
Author(s)
Yurika Ito, Mami Unagami, Fumito Yamabe, Yozo Mitsui, Koichi Nakajima, Koichi Nagao, Hideyuki Kobayashi* (*Responsible Author)
DOI No. 10.1038/s41598-021-89369-z
READ MORE RESEARCH NEWS - MEDICINE
ACADEMICS
Undergraduate Programs
– Medicine
– Pharmaceutical Sciences
– Science
– Nursing
– Health Science
Graduate Programs
–Medicine
–Pharmaceutical Sciences
–Science
–Nursing
Undergraduate Programs
– Medicine
– Pharmaceutical Sciences
– Science
– Nursing
– Health Science
Graduate Programs
–Medicine
–Pharmaceutical Sciences
–Science
–Nursing
RESEARCH
– News
– Guidelines & Policies
– Support Offices
– Facilities
– Security Export Control
Non-Degree Programs
– Clinical Elective Program
– International Physician Observership Program