October 1, 2021
New surgical procedure developed to cure watery eyes
Conjunctivoductivo-dacryocystorhinostomy’ for anastomosis of the conjunctiva and lacrimal duct for intractable canalicular obstruction
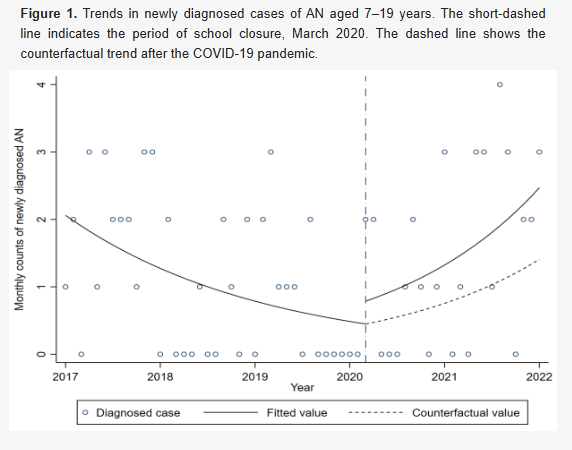
Under normal conditions, tears in the eyes are drained into the
lacrimal sac through small openings called the upper and lower puncta located at the inner corner of the eye (called medial canthus). The tears go through small ducts called the superior and inferior canaliculi and then flow through the lacrimal sac and the nasolacrimal duct, and finally into the nose (Figure A). Obstruction in any part of the above- mentioned passage is the most common cause of watery eyes or epiphora. Epiphora affects the quality of life (QOL) of patients. When both the upper and lower canaliculi are obstructed, the tear fluid cannot be drained into the nose, resulting in epiphora. Although the cause of canalicular obstruction cannot be identified in many cases, it is thought to be associated with aging, trauma, tumors, and oral anticancer medication.
Under normal conditions, tears in the eyes are drained into the
lacrimal sac through small openings called the upper and lower puncta located at the inner corner of the eye (called medial canthus). The tears go through small ducts called the superior and inferior canaliculi and then flow through the lacrimal sac and the nasolacrimal duct, and finally into the nose (Figure A). Obstruction in any part of the above- mentioned passage is the most common cause of watery eyes or epiphora. Epiphora affects the quality of life (QOL) of patients. When both the upper and lower canaliculi are obstructed, the tear fluid cannot be drained into the nose, resulting in epiphora. Although the cause of canalicular obstruction cannot be identified in many cases, it is thought to be associated with aging, trauma, tumors, and oral anticancer medication.
A minor surgery to enlarge the canaliculus by inserting a silicone tube is the common treatment to remove the obstructions. When the canaliculus is reoccluded or cannot be kept open, A Jones tube placement is considered, which semi-permanently places a glass tube that directly connects the nasal cavity and medical canthus. Otherwise, a surgery with an external incision may be considered, which leaves a scar of approximately 2 cm on the side of the nose.
To overcome the disadvantages of these conventional surgical methods, a team of otolaryngologists and ophthalmologists at Toho University Sakura Medical Center has developed a new procedure, ‘conjunctivoductivo-dacryocystorhinostomy.’
All surgical procedures are performed under general anesthesia. First, the entire lacrimal duct and lacrimal sac are
exposed and elevated, and then the lacrimal duct is cut at the lower end (Fig B). At the medial canthus, the conjunctiva is incised (Fig B). The end of the cut lacrimal duct is withdrawn from the conjunctival incision and sutured to form a new lacrimal punctum (Fig C). Then the medial wall of the lacrimal sac is opened wide (Fig C). Now, the former lacrimal duct and lacrimal sac become the new lacrimal passage, and the tear fluid flows in this newly made passage.
The newly developed procedure, ‘conjunctivoductivo-dacryocystorhinostomy’ for the intractable canalicular obstruction does not leave any facial scarring or place foreign matter in the body. We believe that this procedure can help improve the QOL of patients with epiphora,” said Dr. Munetaka Ushio, lead author of the study. The study was published in The Laryngoscope on October 1, 2021.
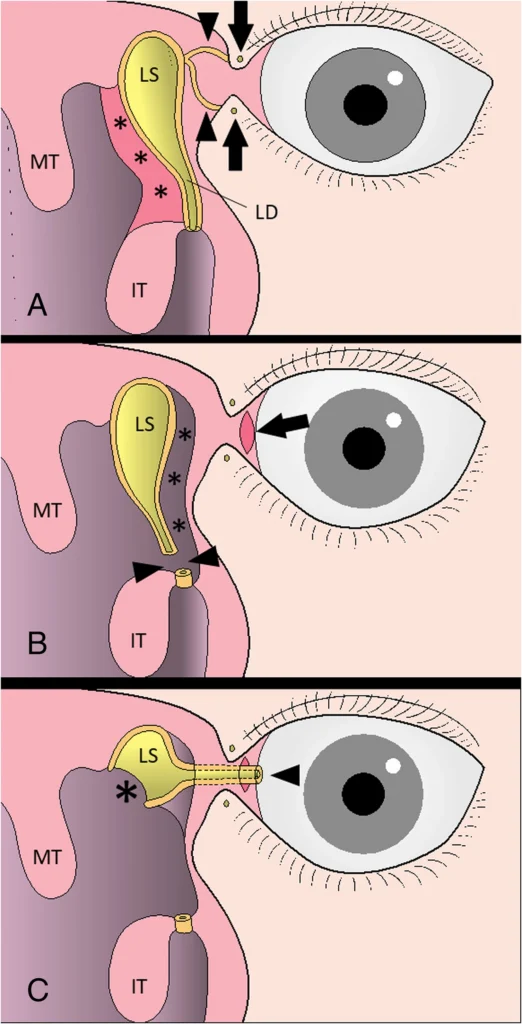
(A) The frontal processes of the maxilla and the lacrimal bone are removed (asterisks) to expose the nasolacrimal duct and the lacrimal sac. The arrows indicate the upper and lower punctum, and the arrowheads indicate the obstructed upper and lower canaliculi. (B) The mucous nasolacrimal duct and the lacrimal sac are elevated from the bony nasolacrimal canal and the orbital periosteum (asterisks). The nasolacrimal duct is then severed at the lower end (arrowheads). The transition from the eyelid to the ocular conjunctiva is incised (arrow). (C) The tip of the severed nasolacrimal duct is withdrawn into and sutured to the conjunctiva incision (arrowhead). The medial wall of the lacrimal sac is trimmed and the lacrimal sac is widely opened (asterisk).
Authors:
Munetaka Ushio, Department of Otolaryngology, Toho University Sakura Medical Center
Hidetaka Masahara, Department of Ophthalmology, Toho University Sakura Medical Center
Masashi Sakamoto, Department of Ophthalmology, Seirei Sakura Citizen Hospital
Yasushi Ohta, Department of Otolaryngology, Toho University Sakura Medical Center
Takatoshi Maeno, Department of Ophthalmology, Toho University Sakura Medical Center
Mitsuya Suzuki, Department of Otolaryngology, Toho University Sakura Medical Center
Munetaka Ushio, Department of Otolaryngology, Toho University Sakura Medical Center
Hidetaka Masahara, Department of Ophthalmology, Toho University Sakura Medical Center
Masashi Sakamoto, Department of Ophthalmology, Seirei Sakura Citizen Hospital
Yasushi Ohta, Department of Otolaryngology, Toho University Sakura Medical Center
Takatoshi Maeno, Department of Ophthalmology, Toho University Sakura Medical Center
Mitsuya Suzuki, Department of Otolaryngology, Toho University Sakura Medical Center
DOI number: 10.1002/lary.29861
READ MORE RESEARCH NEWS - MEDICINE
ACADEMICS
Undergraduate Programs
– Medicine
– Pharmaceutical Sciences
– Science
– Nursing
– Health Science
Graduate Programs
–Medicine
–Pharmaceutical Sciences
–Science
–Nursing
Undergraduate Programs
– Medicine
– Pharmaceutical Sciences
– Science
– Nursing
– Health Science
Graduate Programs
–Medicine
–Pharmaceutical Sciences
–Science
–Nursing
RESEARCH
– News
– Guidelines & Policies
– Support Offices
– Facilities
– Security Export Control
Non-Degree Programs
– Clinical Elective Program
– International Physician Observership Program